Are you looking for signs and symptoms of the most common postpartum complications?
You are in the right place.
In this post, you are going to learn:
- The most common postpartum complications you should know about,
- Early symptoms and warning signs to look out for, and
- When you should call your doctor.
Let’s dive right in.
What is the most common postpartum complication in the immediate postpartum period?
The most common complication in the immediate postpartum period is hemorrhage. This is when you lose an excessive amount of blood after delivering your baby.
Unfortunately, it is the leading cause of maternal death worldwide.
Aside from hemorrhage, other common postpartum complications include:
- Preeclampsia
- Infection, and
- Thombosis or blood clot
Typically, these will all occur in postpartum phase 1.
I’ll go over these in more detail in just a moment.
What is the most common complication of childbirth?
The most common complication of childbirth is a vaginal laceration. This is another way of saying that you develop a tear that can occur in your:
- Vagina,
- Perineum (the area between your vagina and rectum),
- Labia, and/or
- Cervix
Lacerations are very common and occur in about 2/3 of all women who undergo a vaginal delivery.
There are four types of perineal lacerations: first degree, second degree, third degree and fourth degree.
1. A first-degree laceration is superficial, usually incorporating the vaginal mucosa and vaginal tissue. Most can heal on their own, however, if there is a lot of bleeding it will be sutured with stitches.
2. Second-degree lacerations are a little deeper and can damage some muscles of the vagina. These lacerations will be repaired with stitches. Most first time moms will experience this type of laceration.
3. A third-degree laceration is pretty deep and extends from the vagina to the external anal sphincter- the outermost part of your anus. These lacerations require more extensive suturing and skill to repair.
4. Lastly, a fourth-degree laceration extends from your vagina to your rectum. These are relatively rare and require significant repair – often times they need to be done in the operating room. Fourth degree lacerations do have a risk of long term fecal incontinence.
Now let’s go over the major postpartum complications that you don’t want to miss.
The Most Common Postnatal Complications Explained
Postpartum hemorrhage
Postpartum hemorrhage, also known as a PPH, is the leading causes of maternal morbidity and mortality worldwide.
A PPH occurs when there is more than 1000 mL of blood lost during or after a vaginal delivery or cesarean section.
It’s also important to note that a postpartum hemorrhage can occur up to 12 weeks after your delivery. This is what we call a secondary PPH.
A primary PPH occurs within the first 24 hours of delivery whereas a secondary PPH occurs after those first 24 hours and up to 12 weeks after you deliver.
The most common reasons for a postpartum hemorrhage include:
- Uterine atony (where your uterus does not contract as it should following delivery of the placenta)
- Prolonged labor (labors lasting upwards of 18-24 hours)
- Large for gestation baby (the more your uterus is distended, the more likely it wont contract)
- Twins (causing uterine distension due to two babies)
- Retained placenta (placenta should detach within 30 minutes of delivery – if it doesn’t it can continue to bleed)
- Bleeding or coagulation disorders
To treat a postpartum hemorrhage we will:
- Massage your uterus
- Ensure nothing was left inside the uterus like pieces of placenta
- Make sure you do not have a serious tear or laceration from delivery
- Give you medication to contract your uterus
- Possibly place a balloon inside the uterus to control the bleeding
Depending on how severe the blood loss was, you may need to receive a blood transfusion and have a foley catheter placed to monitor your urine output.
If you develop heavy bleeding postpartum – head to an emergency department as soon as possible.
Postpartum Infections
Infections are fairly common postpartum. You can develop an infection in:
- your uterus,
- your urinary tract,
- your breast, or
- your lungs
What are signs of infection after having a baby?
The signs of infection after having a baby are:
- fever >100.4F
- chills
- foul smelling vaginal discharge
- cough
- dysuria or burning with urination
The most common infection is:
Postpartum Endometritis
Endometritis is an infection of the endometrium, the innermost lining of the uterus, that occurs after delivery.
Endometritis can present with:
- fever
- tenderness when your uterus is touched, and/or
- foul smelling vaginal discharge.
If you are experiencing any of these symptoms within a few weeks of delivery you should call your health care provider.
Unfortunately if you’ve had a cesarean section, you are at an even higher risk of postpartum endometritis.
This infection is diagnosed clinically, and will require intravenous or oral antibiotics.
So if you develop a fever postpartum, always call your doctor as you might have an infection.
What Is Postpartum Sepsis?
Sepsis is a very serious condition that can happen after any type of infection.
Your body becomes overwhelmed and has a massive immune response in an effort to fight back.
You are considered septic if you have any of the symptoms below:
- Fever
- Tachycardia or fast heart beat
- Tachypnea or rapid breathing
- Confusion
- Hypotension or low blood pressure
- Oliguria, or not producing adequate urine
- Elevated lactic acid level, determined on a blood sample
Sepsis can be life threatening.
If you experience any of these symptoms call your doctor immediately or go to the nearest emergency department.
Postpartum preeclampsia
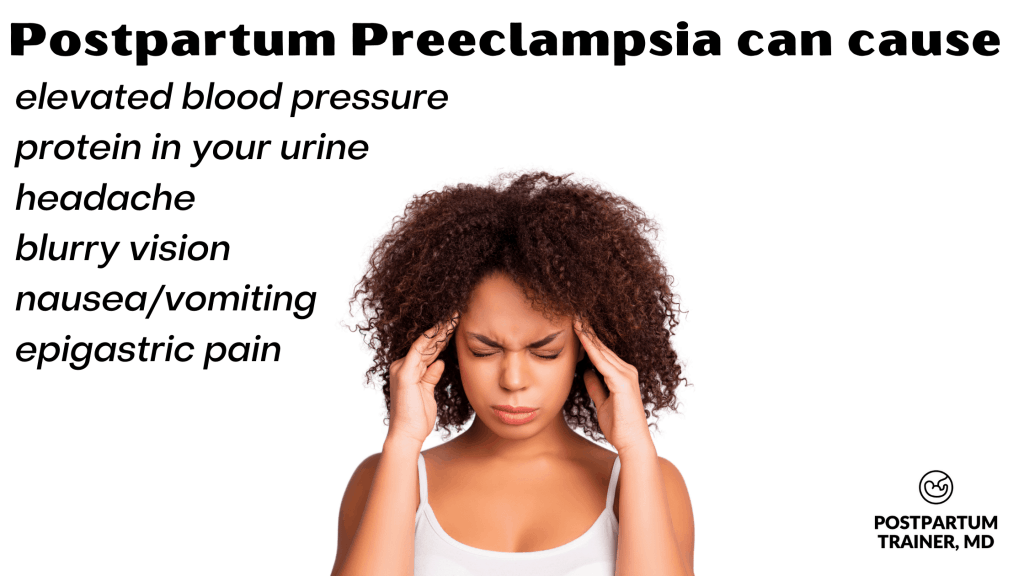
Preeclampsia is a hypertensive disorder of pregnancy that is diagnosed when you have elevated blood pressure (Systolic blood pressure greater than or equal to 140mmHg OR Diastolic blood pressure greater than or equal to 90mmHg) with proteinuria (protein in your urine.)
This can develop during pregnancy, and is diagnosed if you meet the above criteria after 20 weeks of gestation or in the postpartum period.
Aside from elevated blood pressure and proteinuria, postpartum preeclampsia can present with:
- headache
- blurry vision
- nausea and/or vomiting
- abdominal pain, specifically in the right upper quadrant, and/or
- epigastric pain (pain above your belly button
If you are experiencing any of these symptoms you should call your doctor immediately or present to the nearest emergency department.
Preeclampsia is a very serious and life-threatening condition.
It can progress rapidly and develop into stroke, eclampsia which is seizures, and HELLP syndrome which occurs when your liver and platelets become affected.
The treatment of postpartum preeclampsia includes intravenous magnesium sulfate therapy, anti-hypertensives, and very close monitoring of your vital signs.
If you have any of the above symptoms- call your doctor immediately.
Postpartum nausea
Postpartum nausea and vomiting can also be a sign of preeclampsia or HELLP syndrome. If you have these symptoms, check your blood pressure immediately and call your doctor.
If you are found to not have either of these conditions, nausea can occur from eating large meals too soon postpartum.
Do your best to take it slow.
Try eating plain foods like the list I have below, to see how your digestive system does.
- Crackers
- Toast
- Bananas
- Rice
- Fruits
DVT and pulmonary embolism
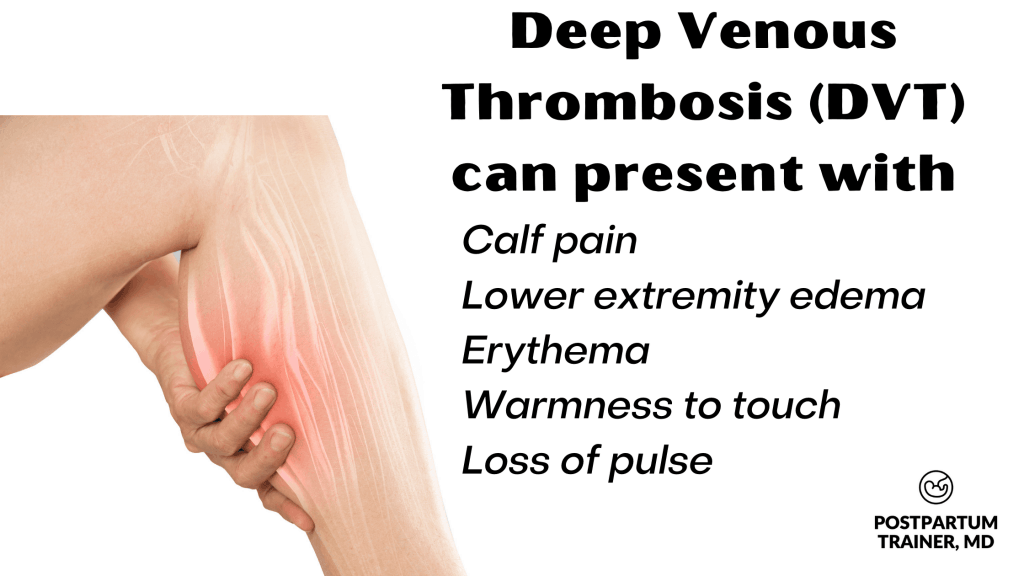
A “DVT” or deep venous thrombosis is a blood clot that forms in one of your lower extremities.
A pulmonary embolism, or “PE” occurs when that blood clot from the lower extremity travels to your lung.
Blood clots AKA venothromboembolisms (VTE) can be extremely dangerous postpartum and increase maternal morbidity and mortality. Unfortunately, pregnancy and postpartum increase the risk of developing blood clots due to the high estrogen environment in your body.
The high estrogen state coupled with decreased activity are the major risk factors for developing postpartum clots.
Symptoms of a DVT can include:
- Pain at your calf
- Swelling in your lower extremity
- Warmness
- Erythema or redness around the area, and/or
- Loss of pulse in the lower extremity
If you have any of these symptoms you should call your doctor immediately or go to the nearest hospital.
To diagnose a DVT you will have a sonogram performed to identify where the blockage is located.
Treatment requires antifibrinolytic therapy usually in the form of a subcutaneous injection with either heparin or lovenox to prevent the clot from traveling to your lungs and causing a PE.
You will most likely need to continue this treatment even after leaving the hospital for a couple of months.
Symptoms of a pulmonary embolism can include:
- Difficulty breathing
- Shortness of breath, and/or
- Rapid heart beat
Again, if you are experiencing any of these symptoms you should call your doctor immediately or go to the nearest hospital.
You will most likely have blood work taken, a chest x-ray, EKG, and CT scan of your chest performed to diagnose and rule out other pathologies.
Treatment is the same and will require antifibrinolytic therapy even after leaving the hospital.
When should I call the doctor postpartum?
You should have a very low threshold when it comes to calling your doctor in the postpartum period. The most common reasons why you should call your doctor include:
- heavy vaginal bleeding
- fever
- elevated blood pressure
- headaches
- changes in vision
- nausea/vomiting
- abdominal pain
- shortness of breath
- rapid heart rate
- signs of postpartum depression
**THIS LIST IS NOT COMPREHENSIVE.**
If you do not feel well, or something doesn’t feel right – seek care right away.
It is always better to call early rather than wait until things have progressed and become very serious.
Other Related Questions
How common is it to die during childbirth?
In the United States, in 2018, there was 17.4 maternal deaths per 100,000 live births.
Non-hispanic blacks are the most at risk population of dying during childbirth, followed by non-Hispanic whites and Hispanic women.
Furthermore, women who are 40 years and over are approximately 8 times more likely to die during childbirth compared to women under the age of 25.
Are there postpartum complications of nursing?
The most common complication of nursing postpartum is mastitis.
Mastitis is an infection of the mammary duct and can occur when one of the milk ducts becomes blocked or a bacteria gets in the milk duct.
This can present with:
- pain in the breast
- fever
- swollen or engorged breast
- warmness at the area
- erythema or redness of the breast
If you are breastfeeding, it is important to continue breastfeeding.
Be sure to call your doctor as you may require oral antibiotics which are also safe for breastfeeding mothers.
What are risk factors for postpartum complications?
If you have preexisting medical conditions or have experienced any of the pregnancy illnesses below you are at an increased risk of postpartum complications.
Some common risk factors include:
- Obesity
- Twin pregnancy
- Gestational diabetes
- Gestational hypertension or preeclampsia
- History of any type of bleeding disorder
- History of postpartum hemorrhage
- History of heart or pulmonary disease
What are the most serious postpartum symptoms not to ignore?
There are several postpartum symptoms you should not ignore.
In fact, I have listed them out for you.
| Heavy vaginal bleeding |
| Headache that does not resolve with tylenol |
| Shortness of breath |
| Change in your vision |
| Severe calf pain |
| Fever |
**AGAIN THIS LIST IS NOT COMPREHENSIVE** IF YOU HAVE ANY DOUBT- BE SURE TO CALL YOUR DOCTOR.
Your body is amazing at nonverbal communication and will give your warning signs, so please do not disregard them!
This may be the first and only prevention warning you will get.
If you have or are currently experiencing any of the aforementioned symptoms please call your doctor or 911 immediately.
Final Words on Postpartum Complications
The postpartum period is a very exciting time as you finally have your baby in your arms, but it can also be a very dangerous time.
It is important you listen to your body and recognize the warning signs and symptoms.
Make sure you follow up at all your postpartum appointments and keep your provider informed of any abnormalities.
Now I want to hear from you.
Did you suffer any complications in the postpartum period?
Comment below and let me know.
Related Articles on Postpartum Complications
- What You Need to Know About Postpartum Activity
- Risks of Exercising Too Soon Postpartum
- Postpartum Exercises You Should Avoid
Get Four Free Workouts To Help Strengthen Your Pelvic Floor & Heal Your Mommy Tummy!

Brittany Robles, MD, MPH, CPT
Brittany Robles is a full-time OBGYN physician, a NASM certified trainer, and a prenatal and postnatal fitness specialist. She holds a Master of Public Health degree in maternal health with a special interest in exercise and nutrition. She is also the co-author of The White Coat Trainer. Learn more about her here.
Sharing is Caring – Send This To A Mom In Need!
